
Catalog Advanced Search
237 Results
-
Contains 19 Component(s) Includes a Live Web Event on 04/22/2026 at 12:00 PM (EDT)
The Maintenance Director Resource is designed to support long-term care facility managers and maintenance directors in developing compliant environmental programs that meet regulatory standards. Registration is free for AHCA/NCAL Members and $65 non-members. For those who are unable to attend live, a recording will be provided to you.
The maintenance director resource is designed to support long-term care facility managers and maintenance directors in building compliant environmental programs that meet regulatory standards.
The Maintenance Director Training Course is structured into four focused modules, each addressing critical areas of facility safety and compliance:
- Maintenance Director Overview
- Fire and Smoke Door Inspection
- Generator Inspection, Testing, and Maintenance
- Portable Patient-Care Related Electrical Equipment (PCREE) Testing
- Kitchen Fire Safety & Compliance
- Oxygen Cylinder Storage
- Sprinkler System ITM
Each module includes educational videos, downloadable PowerPoint presentations, and handouts to support learning and implementation. This training isn’t just informative, it’s compliance-driven.
Upon successful completion, participants receive a certificate that can be used to demonstrate competency in fire and smoke door inspections, fulfilling annual requirements under NFPA 80 and NFPA 105, as part of the 2012 Life Safety Code®.
Whether you’re looking to train new staff or reinforce existing protocols, this course offers flexible learning options. Modules can be completed individually or as a full series, allowing facilities to tailor the experience to their specific needs.
Cost: Free for AHCA/NCAL Members | $65 non-members
No CEs awarded upon completion.
Instructions to Register:
- For optimal performance, please use the latest version of Chrome, Firefox, Edge, or Safari 14+.
- Members will need to log in using their existing email and password first.
- Once you are logged in to the website, you will be able to register by clicking the green register button at the top right of the page.
- If you have forgotten your password, click here.
- If you are new to the site, you can create an account here. Answer all fields on the 'Create an Account' page, especially when locating your company name. You can search by name or zip code. After creating an account, you will be able to register.
- If you are unsure if you are a member of AHCA, you can email update@ahca.org to confirm your membership status.
Instructions to Begin, after registering:
- To begin the training, click on the Contents tab.
- Participants can move throughout the lessons in the course by clicking on the header of each module to expand or minimize their view.
Email educate@ahca.org if you need technical assistance. Questions regarding Life Safety and Emergency Preparedness, or this training, please email EmergencyPrep@ahca.org
© 2025 American Health Care Association. All rights reserved. Materials subject to this copyright may be photocopied or distributed for nonprofit or educational advancement. The use, photocopying, and distribution for commercial purposes of any of these materials is expressly prohibited without the prior written permission of the American Health Care Association
-
Register
- Non-member - $65
- Member - Free!
- *Further discounts may apply once you log in.
- More Information
-
Contains 2 Component(s) Includes a Live Web Event on 03/25/2026 at 2:00 PM (EDT)
This webinar will share practical insights on how profession-based learning partnerships can support nursing teams, enhance care delivery, and build sustainable workforce pipelines. Registration is free to AHCA/NCAL members. If you are not able to attend live, the recording will be provided to you.
Long term care (LTC) leaders are seeking practical ways to strengthen CNA pipelines and other LTC positions while preserving care quality, culture, and resident experience. Hear from AHCA/NCAL state affiliates, providers and other leaders on how HOSA (Future Health Professionals) and CAPS can help foster meaningful LTC partnerships in your communities.
AHCA/NCAL’s state affiliates of Florida and Arizona have engaged in successful partnerships with HOSA. Learn more about the meaningful connections that are being made in those states on getting youth involved in the sector. We will also be joined by a provider from Friendship Village who has just begun judging Arizona HOSA competitions and his perception of how significantly this relationship can potentially assist his center grow their workforce. Next, you will learn about a successful partnership between Cedar Falls CAPS and Western Home Communities in Iowa that brings students into authentic caregiving environments early. Through this collaboration, students build durable nursing skills, develop meaningful relationships with residents, and participate in an embedded CNA pathway aligned to Western Home’s care philosophy and workforce needs. Nursing teams benefit from better-prepared candidates, stronger culture fit and reduced onboarding friction—while residents gain purposeful intergenerational connection. Together, this webinar will share practical insights on how profession-based learning partnerships can support nursing teams, enhance care delivery, and build sustainable workforce pipelines.
Learning Outcomes:
- Better understand the value of youth engagement partnerships.
- Explore potential engagement opportunities and connections.
- Get your pressing questions answered on students in the caregiving environment.
Presenters:
- Kristen Knapp, Senior Director of Strategy & Communications, Florida Health Care Association
- Jeff Barrett, Director of Workforce and Leadership Development, Arizona Health Care Association
- Jason Bishop, Director of Facilities at Friendship Village in Tempe, Arizona
- Nate Clayberg, CEcD, Business and Industry Director with the CAPS Network
- Ethan Wiechman, Director of Cedar Falls CAPS
- Krista Dreyer, Director of Education
- Lisa Ridder, Regional Director of Quality and Clinical Services
- Wendy Ager, Chief Clinical Officer
- Darrell McCormick, Chief Operating Officer
- Jerry Harrs, President- Cedar Falls Operations
Registration is free to AHCA/NCAL members.
If you are not able to attend live, the recording will be provided to you.
Instructions to Register:
- To avoid technical problems, use Google Chrome.
- Members will need to log in using their existing email and password first.
- Once you are logged in to the website you will be able to register by clicking the green register button at the top of the page.
- If you have forgotten your password click here.
- If you are new to the site, you can create an account here. Answer all fields on the create an account page- especially locating your company name. You can search by name or zip code. After creating an account, you will be able to register for the webinar.
Instructions to join, after registering:
- On the day of the webinar, you will be able to join 15 mins before.
- Log in and return to the contents page to open the webinar.
Email educate@ahca.org if you need assistance.
-
Register
- Member - Free!
- *Further discounts may apply once you log in.
- More Information
-
Contains 11 Product(s) 1 new product(s) added recently
During this series, hear directly from provider members – including AHCA/NCAL workforce committee members – and other experts on these matters on what has and hasn’t worked from their experiences. It is also an opportunity to get your pressing questions answered. Registration is free to AHCA/NCAL members. Each webinar will be recorded.
AHCA/NCAL is holding a webinar series this year focused on workforce related matters impacting our long term care providers across the country. This series is focused on issues from career ladders to getting more youth interested in the long term care field to hiring immigrants and refugees. During this series, hear directly from provider members – including AHCA/NCAL workforce committee members – and other experts on these matters on what has and hasn’t worked from their experiences. It is also an opportunity to get your pressing questions answered.
Registration is free to AHCA/NCAL members.
If you are not able to attend live, the recording will be provided to you. A certificate of attendance will be available after webinar. (No CEs)
Webinar's in this series will include:
- Interested in an Apprenticeship Partnership?
- Building the Path: Creating Careers in Long Term Care
- Refugee Workforce Partnerships in Long Term Care
- Career Upskilling: Creating Opportunities to Level Up
- Key Strategies for Retaining Your LTC Workforce
- Building Employee Resiliency through Person-Centered Approaches
- Why Registered Apprenticeship? How It CAN Help Build Your LTC Workforce
- Inspiring the Next Generation: Engaging Youth in Long Term Care: Part 1
- Resource: How To Guide: Hosting a Facility Tour
- Inspiring the Next Generation: Engaging Youth in Long Term Care: Part 2:
- Building Resilient Teams Through Cross-Training: Strategies, Challenges, and Success Stories
- Where Students and Community Meet: Transforming Workforce and Resident Experiences Together
Follow the Instructions Below to Register:
- To avoid technical problems, use Google Chrome.
- Members will need to log in using their existing email and password first.
- Once you are logged in to the website you will be able to register by clicking the green register button at the top of the page.
- If you have forgotten your password click here.
- If you are new to the site, you can create an account here. Answer all fields on the create an account page- especially locating your company name. You can search by name or zip code. After creating an account, you will be able to register.
Email educate@ahca.org if you need assistance.
STATEMENT OF AHCA/NCAL’S ARTIFICIAL INTELLIGENCE (AI) POLICY
To foster an environment of candor and the open exchange of ideas, AHCA/NCAL prohibits the recording of meetings by attendees. This includes but is not limited to any use of artificial-intelligence tools or assistants that record and transcribe information. AHCA/NCAL has the right to immediately remove AI tools or assistants present on calls and placed by attendees.
© 2025 American Health Care Association. All rights reserved. Materials subject to this copyright may be photocopied or distributed for the purpose of nonprofit or educational advancement. The use, photocopying, and distribution for commercial purposes of any of these materials is expressly prohibited without the prior written permission of American Health Care Association.
-
Register
- Member - Free!
- More Information
-
Contains 54 Component(s), Includes Credits Includes Multiple Live Events. The next is on 03/16/2026 at 1:00 PM (EDT)Extended Sale Now through March 7th!
The Leadership Academy exists to equip leaders in Long Term Care and Assisted Living facilities with trust-building knowledge, skills, and practices to enhance patient safety, staff well-being, and the daily functioning of the facility. This virtual, interactive leadership development academy provides tools and strategies to build trust, strengthen teams, and improve outcomes across their organizations. Cost: $975 for AHCA Members $1175 for Non-Members
Discount Extended!
Use discount code Leader2026 to save $100 off registration fees! Now through March 7th, 2026
The Leadership Academy exists to equip leaders in Long Term Care and Assisted Living facilities with trust-building knowledge, skills, and practices to enhance patient safety, staff well-being, and the daily functioning of the facility.
This virtual, interactive leadership development academy provides tools and strategies to build trust, strengthen teams, and improve outcomes across their organizations.
Leadership Academy Participants Will Learn to:
- Assess the presence of trust in your facility
- Foster a culture of psychological safety
- Address resistance to change and misinformation
- Build trust through active listening and motivational interviewing
- Promote staff wellbeing and engagement
- Identify the impact of inequities in building trust
- Use motivational interviewing techniques
What to Expect:
- Virtual 17-week program The first session kicks off March 16th! Save your calendar!
- Bi-weekly 1-hour commitment
- Live sessions, practice reflections, and peer collaboration
Cost:
$975 for AHCA Members
$1175 for Non-MembersThis program offers up to 24.75 NAB-Approved CE credits for administrators and 24.75 contact hours for nurses. Please note, nurses are individually responsible for submitting the necessary documentation to verify continuing education completion for license renewal
Jerald Cosey, NHA
Kate B. Hilton, JD, MTS
Lindsay Martin, MSPH
Courtney Bishnoi, VP AHCA
David Gifford, MD, AHCA
Darius McDonald, TN Health Care Association
Please use Google Chrome for the best user experience.
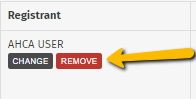
One individual can purchase multiple registrations for more participants by adding them to their cart during the checkout process. Please note, for this option to work, every participant will need to have an ahcancalED account first AND have been signed in to the website at least once.
To add several participants, please click the green button in the cart that says:
 .
.
You will then be able to search for more than one participant using their email address. If the person making payment should not have access to the course, then you can remove yourself by clicking the red "remove" button by your name.
*Payment Tip: The price of the training will be based on each registrant’s member type (member or non-member). please be sure when you are paying with a credit card the bill-to and shipping address are the same*
If you need assistance, please email educate@ahca.org
-
Register
- Non-member - $1,175
- Member - $975
- *Further discounts may apply once you log in.
- More Information
-
Contains 2 Component(s) Includes a Live Web Event on 03/10/2026 at 2:00 PM (EDT)
Join this free 60-minute presentation discussing modern dining and complementary wellbeing practices for senior living residents. Registration is free to everyone. CEs: Approval from ANFP for 1 CE for CDMs
Modern dining approaches in senior living embrace whole-person practices of care. Today’s modern communities focus on individualized preferences utilizing menu options, flexible dining times, restaurant-quality recipes, and a health-forward focus that optimizes the resident experience. Complementary wellbeing programming focusing on lifestyle enrichment can enhance nutritional status and bolster safeguards around malnutrition and advancing chronic disease.
Join this free 60-minute presentation discussing modern dining and complementary wellbeing practices for senior living residents. Learning objectives include:
- Understand how modern dining approaches enhance resident experience and help in retaining census
- Be able to describe how dining programs directly affect resident risk of malnutrition & chronic disease
- List three ways that upgrading menus, recipes, dining options and plate presentation can enhance resident satisfaction
- Understand the interconnectedness between wellbeing lifestyle programming, nutrition, and resident outcomes
- Be able to discuss the nuance of the new Dietary Guidelines as they relate to nutrition for older adults
Faculty:
Jen Bruning, MS, RDN, LDN, Senior Director of Partner Education for Incite Strategic Partners
Linda Ricco, Vice President of Healthcare Solutions for TCM Consulting & Management
CEs: Approval from ANFP for 1 CE for CDMs
Registration is free to AHCA/NCAL members and non-members.
If you are not able to attend live, the recording will be provided to you.
Instructions to Register:
- To avoid technical problems, use Google Chrome.
- Members will need to log in using their existing email and password first.
- Once you are logged in to the website you will be able to register by clicking the green register button at the top of the page.
- If you have forgotten your password click here.
- If you are new to the site, you can create an account here. Answer all fields on the create an account page- especially locating your company name. You can search by name or zip code. After creating an account, you will be able to register for the webinar.
Instructions to join, after registering:
- On the day of the webinar, you will be able to join 15 mins before.
- Log in and return to the contents page to open the webinar.
Email educate@ahca.org if you need assistance.
-
Register
- Non-member - Free!
- Member - Free!
- More Information
-
Contains 11 Component(s)
Surveys can be a highly anxious time, especially for staff in long-term care facilities. The AHCA Survey, Regulatory committee, created the Preparing Staff for Survey toolkit to provide quick, easy to use, Tip Sheets for training staff on the survey process. Included in the toolkit is a video to introduce staff to long-term care surveys, and individual tip sheets to provide to new staff, current staff, and specific disciplines. There is also a tip sheet included to prepare staff for surveyor interviews and infection control practices. By providing the training on what to expect, during a survey, buildings can educate staff, so they are better prepared for surveys. Registration is open to AHCA provider members.
Surveys can be a highly anxious time, especially for staff in long-term care facilities. The AHCA Survey, Regulatory committee, created the Preparing Staff for Survey toolkit to provide quick, easy to use, Tip Sheets for training staff on the survey process. Included in the toolkit is a video to introduce staff to long-term care surveys, and individual tip sheets to provide to new staff, current staff, and specific disciplines. There is also a tip sheet included to prepare staff for surveyor interviews and infection control practices. By providing the training on what to expect, during a survey, buildings can educate staff, so they are better prepared for surveys.
Registration is open to AHCA provider members.
- To avoid technical problems, use Google Chrome.
- Members will need to log in using their existing email and password first.
- Once you are logged in to the website you will be able to register by clicking the green register button at the top of the page.
- If you have forgotten your password click here.
- If you are new to the site, you can create an account here. Answer all fields on the create an account page- especially locating your company name. You can search by name or zip code. After creating an account, you will be able to register.
Email educate@ahca.org if you need assistance.
The learner must review the introduction video before advancing to the downloadable materials. A certificate of completion is available upon completion.
© 2024 American Health Care Association. All rights reserved. Materials subject to this copyright may be photocopied or distributed for the purpose of nonprofit or educational advancement. The use, photocopying, and distribution for commercial purposes of any of these materials is expressly prohibited without the prior written permission of American Health Care Association.
-
Register
- Member - Free!
- More Information
-
Contains 8 Component(s)
These resources provide a structured, practical framework for understanding CoreQ, ensuring accurate data submission, and leveraging satisfaction insights to support continuous quality improvement. For more information about CoreQ, please visit the CoreQ website. Registration is free to AHCA/NCAL members.

The CoreQ Toolkit is now available on ahcancalED. Developed to support providers, vendors, and state affiliates, this comprehensive set of tools equips organizations with the knowledge and practical guidance needed to successfully participate in CoreQ and use customer satisfaction data to drive quality improvement.
CoreQ plays an important role in measuring customer satisfaction across post-acute and long term care settings. Whether you are new to CoreQ or looking to strengthen your processes, these resources are designed to provide clarity, streamline data submission, and support meaningful use of results.
The collection includes a CoreQ Overview to introduce the purpose and structure of the program, along with Debunking CoreQ Myths to address common misconceptions about participation, data submission, and public reporting. Together, these foundational resources help organizations build confidence and shared understanding around CoreQ.
For those preparing to submit data, the collection features step-by-step guidance for both providers and approved vendors. The CoreQ Vendor Upload Instructions outline technical requirements, file specifications, and best practices to ensure accurate submission. The How to Upload to CoreQ guide walks providers through accessing the system, submitting data, confirming acceptance, and avoiding common errors.
To support education and consistent messaging, the CoreQ Stock Slides offer ready-to-use presentation materials for trainings, meetings, and affiliate events. The Questions & Responses resource provides clear, concise answers to frequently asked questions related to scoring, timelines, participation requirements, and reporting.
In addition, the Focusing on Customer Satisfaction on Your Quality Award Journey resource highlights how CoreQ data can strengthen performance improvement efforts and support a culture of customer-centered care. It offers strategies for using satisfaction results to engage staff, inform decision-making, and demonstrate excellence throughout the Quality Award journey.
Together, these resources provide a structured, practical framework for understanding CoreQ, ensuring accurate data submission, and leveraging satisfaction insights to support continuous quality improvement. For more information about CoreQ, please visit the CoreQ website: CoreQ - satisfaction among patients, residents, and their families
Registration is free to AHCA/NCAL members.
Questions about the toolkit may be sent to research@ahca.org. Technical assistance may be directed to educate@ahca.org.
-
Register
- Member - Free!
- *Further discounts may apply once you log in.
- More Information
-
Register
-
Contains 9 Component(s)
This series is designed to equip facilities with the knowledge needed to confidently implement and respond to these regulatory updates. registration is free for Members and $65 for non-members.
Join us for a comprehensive 4-part webinar series exploring the recent updates to the State Operations Manual. This series is presented by members of the AHCA Regulatory team, who will guide you through the most significant changes and their impact on providers.
Across four focused sessions, we will break down the key revisions and offer practical insights to help you navigate the updated requirements:
- Part 1: Introduction to the overall updates and a detailed review of the changes made to Chapter 5.
- Part 2: An overview of the newly added/updated definitions in Chapter 7, along with important updates related to Nursing Waivers and Life Safety Code (LSC) Waivers.
- Part 3: A deep dive into the extensive changes to the survey process, including what providers can expect moving forward.
- Part 4: A review of updates affecting IJ determinations, IDRs, and CMPs, including procedural and operational impacts.
This series is designed to equip facilities with the knowledge needed to confidently implement and respond to these regulatory updates.
Cost:
Free for Members and $65 for non-members
Instructions to Register:
- To avoid technical problems, use Google Chrome.
- Members will need to log in using their existing email and password first.
- Once you are logged in to the website you will be able to register by clicking the green register button at the top of the page.
- If you have forgotten your password click here.
- If you are new to the site, you can create an account here. Answer all fields on the create an account page- especially locating your company name. You can search by name or zip code. After creating an account, you will be able to register.
Instructions to Begin, after registering:
- To begin the training, click on the Contents tab.
- Participants can move throughout the course by clicking on the header of each module to expand or minimize their view.
Questions? Email educate@ahca.org
-
Register
- Non-member - $65
- Member - Free!
- *Further discounts may apply once you log in.
- More Information
-
Contains 6 Component(s)
Through these realistic interactions, participants will explore how everyday moments—such as service delays, unmet expectations, or miscommunication—can either escalate frustration or become opportunities to reinforce empathy, professionalism, and teamwork. Registration is free to AHCA/NCAL members.

CEC Customer Service Management Subcommittee
The Turning Tension into Trust team training program is now available on ahcancalED. Developed by and for long term care providers, this customer experience and satisfaction resource equips frontline staff and leaders with practical skills to navigate challenging interactions, strengthen relationships, and build trust with residents, families, and colleagues.
In today’s long term care environment, moments of tension are inevitable. How teams respond in those moments can significantly impact satisfaction, trust, and overall perception of care. This program focuses on transforming difficult situations into opportunities for connection, understanding, and improved outcomes through effective communication and teamwork.
Part 1 of the training is now available and centers on real-life customer experience scenarios involving internal frontline departments, including front desk/reception, dining services, recreation and activities, and housekeeping. These scenarios reflect common, day-to-day interactions where tension may arise and where staff responses play a critical role in shaping trust, satisfaction, and overall perception of care.
Through these realistic interactions, participants will explore how everyday moments—such as service delays, unmet expectations, or miscommunication—can either escalate frustration or become opportunities to reinforce empathy, professionalism, and teamwork.
Part 1 of this training consists of five scenario scripts, each designed to build practical, applicable skills, and facilitate open discussion amongst team members. Each scenario explores the foundations of customer experience in LTC, the common sources of conflict and dissatisfaction, and proven strategies to prevent escalation and resolve concerns. Participants will learn how to recognize emotional cues, respond with empathy, and apply consistent approaches that support a positive care experience. Each scenario may be completed independently or together as a comprehensive team-based learning program.
Across all scenarios in Part 1, the training emphasizes four core focus areas, which serve as common themes throughout the program:
- Awareness and empathy – understanding perspectives, emotions, and expectations
- Communication and listening – using clear, respectful, and effective communication techniques
- De-escalation and service recovery – managing tension, addressing concerns, and restoring trust
- Team alignment and consistency – reinforcing shared values and coordinated responses across roles
Each focus area builds on the previous one, helping teams develop confidence and consistency when navigating high-emotion situations across departments.
Registration is free to AHCA/NCAL members.
Questions about the resource may be sent to research@ahca.org. Technical assistance may be directed to educate@ahca.org.
-
Register
- Member - Free!
- *Further discounts may apply once you log in.
- More Information
-
Contains 2 Component(s)
The guide is organized to support both new and experienced social media users, with clear sections that make it easy to reference best practices. Registration is free to AHCA/NCAL members.
CEC Social Media Management Subcommittee
Effective social media management is essential for senior living communities to engage residents, families, and staff while protecting your community’s reputation. This new resource, Social Media Management for Senior Living: Tips and Best Practices, provides practical guidance for creating a positive, professional, and consistent online presence.
Designed for leaders, marketing teams, and frontline staff who interact with social media, this resource covers key strategies for:
- Crafting meaningful content that highlights community life, programs, and resident stories while maintaining privacy and dignity.
- Engaging families and prospective residents through thoughtful, transparent, and timely communication.
- Managing challenging situations online with professionalism, empathy, and de-escalation techniques.
- Aligning team communication so all staff represent your community consistently across platforms.
Whether your community is just getting started with social media or looking to refine existing practices, this resource offers actionable tips, best practices, and real-world examples to help your team communicate confidently and effectively. By following these guidelines, senior living communities can strengthen trust, enhance engagement, and create a positive, welcoming online environment that reflects the high-quality care and service residents and families expect.
Resource Structure
The guide is organized to support both new and experienced social media users, with clear sections that make it easy to reference best practices:
Table of Contents:
- Overview (p.1) – An introduction to the importance of social media in senior living and its impact on resident satisfaction, family engagement, and community reputation.
- Common Terminology Used in Social Media Management (pp.2–3) – Key terms and concepts every staff member should understand to navigate social platforms effectively.
- Promoting Positive Engagement (pp.4–6) – Strategies for sharing meaningful content, highlighting community life, and creating opportunities for interaction online.
- Responding to Negative Feedback (pp.7–9) – Guidance on addressing complaints or criticism respectfully, maintaining professionalism, and protecting your community’s trust.
- DOs and DON’Ts for Senior Care Social Media (pp.10–12) – Practical tips on what to post, what to avoid, and how to maintain privacy and dignity while representing your community.
- Case Studies (pp.13–16) – Real-world examples that illustrate best practices, lessons learned, and successful approaches to social media management in senior living.
- Federal Government Enforcement (p.16) – An overview of relevant regulations and legal considerations to help your community stay compliant while engaging online.
Whether your community is just getting started with social media or looking to refine existing practices, this resource provides actionable guidance, clear examples, and step-by-step strategies to help your team communicate confidently and effectively.
By following these guidelines, senior living communities can strengthen trust, enhance engagement, and create a positive, welcoming online environment that reflects the high-quality care and service residents and families expect.
Registration is free to AHCA/NCAL members.
Questions about the resource may be sent to our Social Media Manager. Technical assistance may be directed to educate@ahca.org.
-
Register
- Member - Free!
- *Further discounts may apply once you log in.
- More Information
