
Abuse Alert Icons on Nursing Home Compare: What You Need to Know
On October 7, the Centers for Medicare & Medicaid Services (CMS) announced that starting October 23, 2019, Nursing Home Compare (NHC) will flag skilled nursing centers that have been cited for abuse, neglect and exploitation with an alert icon. Facilities that receive an alert icon will also have the survey component of their star rating capped at 2 stars.
A nursing center will receive an alert icon on NHC if it falls under one of two categories:
- If a nursing center has been cited for abuse that led to harm (G or above) in the last year for one of three abuse F-tags; or
- If a nursing center has been cited for abuse with the potential for harm (D and above) in each of the last two years for one of three abuse tags.
Note: a survey cycle is defined by the standard survey and a rolling 12-month time window. As such, Cycle 1 is comprised of the most recent standard survey and any complaint survey in the 12 months prior to data release (months 1 through 12). Cycle 2 is comprised of the prior standard survey and any complaint surveys during the previous 12-month window (13 to 24 months prior to data release).
The three abuse and neglect citations that will result in an icon are as follows:
- F600: Free from abuse and neglect
- F602: Free from misappropriation/exploitation
- F603: Free from involuntary seclusion
Note that CMS is also using F223 and F224, which were the abuse F-tags prior to renumber of tags in 2017.
After a nursing center has been free from any of these three citations (at any level) for a full year and inspection cycle, the icon will be removed. The NHC website will be updated with new information on a monthly basis. If you have any questions, please contact the AHCA Regulatory team at regulatory@ahca.org.
Communication Resources Available
-
Contains 3 Component(s)
This toolkit includes: Talking Points, Template Letter for Families, Template Letter for Referral Sources/Payors
Click the
 button found in the upper right corner of your screen
button found in the upper right corner of your screen OR
Follow these three easy steps below!
Step 1
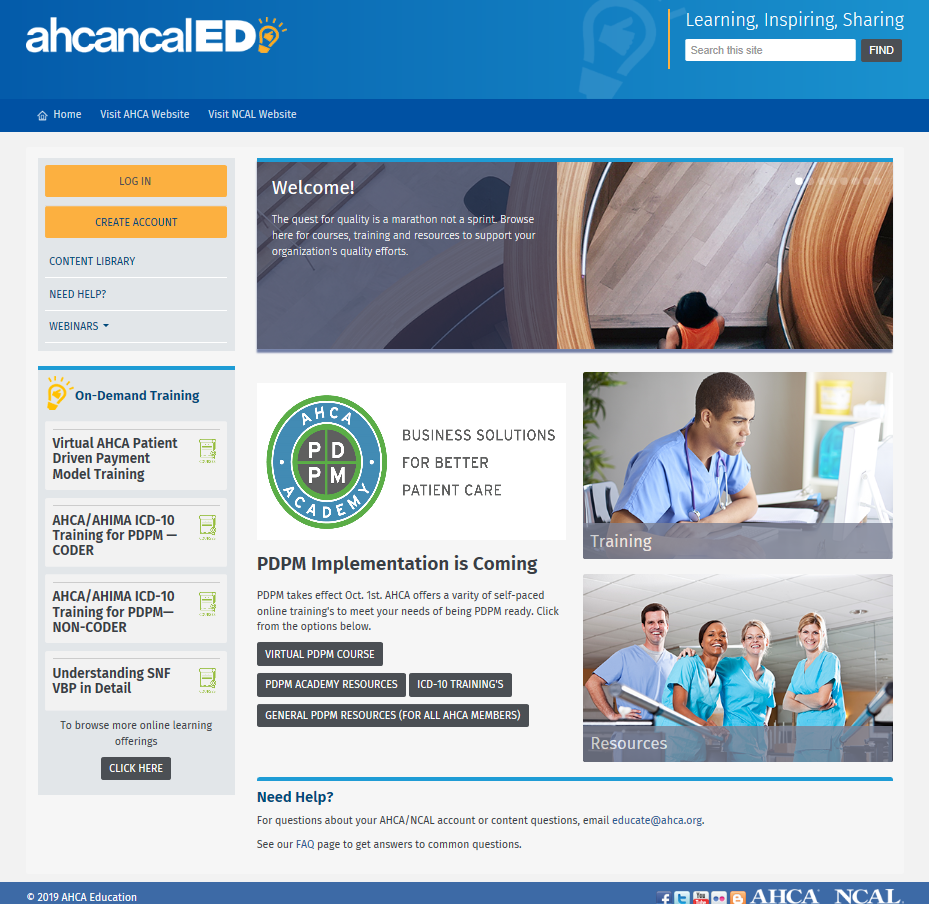
Click the orange log in button in the upper left hand corner.
Use your user name and password that you would use for LTC Trend Tracker or the AHCA NCAL website.
Don’t have an account or can’t remember?
Click the CREATE ACCOUNT button.
Non-members can create an account with your first, last name and email.
AHCA/ NCAL Members - *Please note* you must add your member facility name to your login
Once you are in and can see your name in the upper left hand corner, you are ready to go!
Step 2
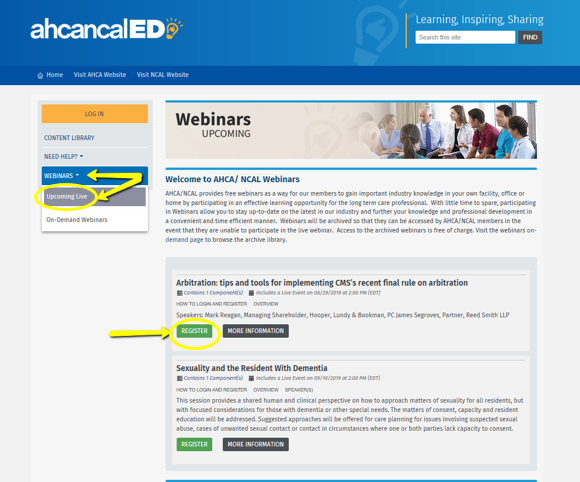
From the home page click on a category (Resources, Training, Webinars or On-Demand Training) For this demonstration, let’s try Webinars- Upcoming Live.
On the “upcoming webinars” page go to a product in which you are interested. Click the green REGISTER button.
Or click the title of the webinar and you will be redirected to the page where you can view the overview, handouts or resources associated with that product. You can also click REGISTER in the upper right hand corner. The content will be available in your dashboard.
Step 3
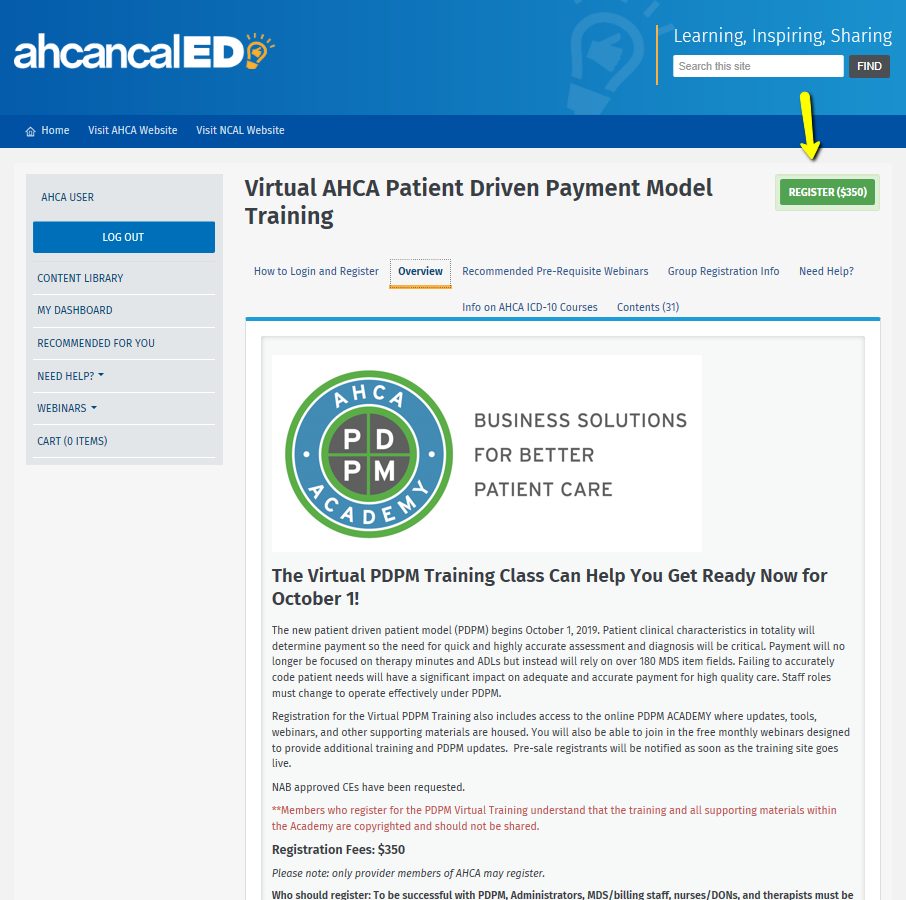
Almost there!
If the resource you are trying to access is a paid-for product, fill out the registration details and voila! The products are yours to use and can be found in your dashboard.
Need further help? Email us at educate@ahca.org
We’ll walk you through it.
This toolkit includes:
- Talking Points
- Template Letter for Families
- Template Letter for Referral Sources/Payors
© 2022 American Health Care Association. All rights reserved.
All Communication Tools materials subject to this copyright may be photocopied or distributed for the purpose of nonprofit or educational advancement. The use, photocopying, and distribution for commercial purposes of any of these materials is expressly prohibited without the prior written permission of American Health Care Association.
-
Register
- Member - Free!
- More Information
AHCA/NCAL Education Resources
-
Contains 3 Component(s)
It is critical for nursing centers and assisted living communities to address and mitigate resident-to-resident occurrences or potential incidents of resident-to-resident mistreatment. While mistreatment may or may not meet the definition of abuse, it would include negative and aggressive physical, sexual, or verbal interactions between long-term care residents that is unwelcome and have high potential to cause physical or psychological distress in the recipient.
It is critical for nursing centers and assisted living communities to address and mitigate resident-to-resident occurrences or potential incidents of resident-to-resident mistreatment. While mistreatment may or may not meet the definition of abuse, it would include negative and aggressive physical, sexual, or verbal interactions between long-term care residents that is unwelcome and have high potential to cause physical or psychological distress in the recipient.
Objectives:
- Conduct a thorough investigation with proper documentation, follow up, and monitoring and care planning as needed.
- Create a structured self-assessment process to address the resident-to-resident occurrence and minimize or mitigate similar events for all residents. This includes a need to:
- Document immediate interventions;
- Conduct a root cause analysis process to identify the specific/source, root cause or causal factor of the problem; and
- Identify future actions to ensure sustained efforts to identify and prevent potential resident-to-resident mistreatment.
- Identify existing AHCA/NCAL resources to support providers in addressing resident-to-resident mistreatment.
Note: These tools were developed by members of AHCA/NCAL’s Survey/Regulatory Committee to assist centers and communities in addressing adverse events and potential adverse events, documenting and tracking the steps they have taken, and identifying best practices for ongoing improvement. Use of these tools does not guarantee regulatory compliance nor mitigate potential liability. Providers should adapt their tools, policies, and processes as needed to ensure compliance with current federal and state requirements and use both professional judgement and the advice of legal counsel in determining whether or how to share these mitigation tools.
© 2022 American Health Care Association. All rights reserved.
All Provider Self-Assessment and Mitigation Tools for Resident to Resident Occurrences materials subject to this copyright may be photocopied or distributed for the purpose of nonprofit or educational advancement. The use, photocopying, and distribution for commercial purposes of any of these materials is expressly prohibited without the prior written permission of American Health Care Association.
-
Register
- Member - Free!
- More Information
-
Contains 5 Component(s)
A Framework for Successful Clinical Outcomes
Success in achieving positive resident/patient outcomes is even more critical now than ever before. The link between quality and payment in long term and post-acute care is growing stronger, as evidenced by the SNF Value Based Purchasing Program (VBP), Improving Post-Acute Care Transformation (IMPACT) Act, SNF Quality Reporting Program (QRP) and more. In addition, regulatory activity is intensifying through focused surveys on adverse events, dementia care and MDS. The Five-Star Rating system and Nursing Home Compare have been revised and will add items in the future as it broadens public reporting and transparency. Most importantly, consumers expect and deserve high quality care.
The Association’s Clinical Practice Committee designed a framework series that outlines guiding elements such as individualized care approaches, effective transitions of care, QAPI concepts, safety, risk management, team-based care, and diagnostic quality. Care providers that use these resources can more effectively apply knowledge through organizational approaches and clinical care that leads to optimal patient outcomes and quality of life.
We hope you find this Series useful to your practice to improve lives of the individuals who stay and live in centers across the nation.
© 2022 American Health Care Association. All rights reserved.
All Building Prevention into Every Day Practice materials subject to this copyright may be photocopied or distributed for the purpose of nonprofit or educational advancement. The use, photocopying, and distribution for commercial purposes of any of these materials is expressly prohibited without the prior written permission of American Health Care Association.
Holly Harmon, RN, MBA, LNHA, FACHCA
Senior VP, Quality, Regulatory & Clinical Services
American Health Care Association
Holly Harmon, RN, MBA, LNHA, FACHCA brings both passion anda wealth of practical, real-world, clinical and operational experience to herrole as Senior Director of Clinical Services at AHCA. Her extensive service ina wide array of settings including post-acute care, long term care, residentialcare, assisted living, independent living, a psychiatric hospital andoccupational health have provided her with insights, knowledge, skills andinnovative ideas which she exuberantly shares with others.
In addition to her vast clinical experience, Ms. Harmon hasput her dynamic energy into leading the statewide Maine Culture ChangeCoalition/LANE as President, the Maine Partnership to Improve Dementia Care inNursing Homes as Co-Chair, Vice-President of American College of Health CareAdministrators, Maine Chapter and the Maine LANE Co-Convener for the nationalAdvancing Excellence in America’s Nursing Homes Campaign. She also served asthe Director of Quality Improvement & Regulatory Affairs at the MaineHealth Care Association.
She puts her boundless energy and warm and energeticpersonality into training, education and presenting both, nationally andlocally. She has made simplifying the complex world of long term and post-acutecare policy and practice an art.
Diane Vaughn, RN, C-DONA/LTC, LNHA
Diane has over 37 years as a RN including experience in hospitals, ICF-MR, Skilled Care, and Assisted Living. She has been a staff nurse, nurse manager, nurse educator, director of nursing , quality manager, assistant administrator, and national consultant. She is licensed as a NHA since 2003. She is a national speaker on leadership, LTC quality and nursing home regulatory issues, an accredited QIS instructor, and an endorsed parish nurse.
Dr. Anna Fisher, DHA, CMDCP, CDP
Director of Quality and Education
Hillcrest Health Services
Dr. Anna Fisher, DHA, CMDCP, CDP, is a Certified Montessori Dementia Care Practitioner and Director of Quality & Education at Hillcrest Health Services and is responsible for quality and education services for assisted living, memory support, adult day services, in-patient rehabilitation, outpatient therapy, home health care, private duty, telehealth, hospice, and skilled nursing care. She is also an adjunct professor in the College of Arts and Sciences at Bellevue University.
Dr. Fisher is a Clinical Practice Committee Member, Emergency Preparedness Committee Member, and Silver Quality Award Senior Examiner for the American Health Care Association (AHCA) / National Center for Assisted Living (NCAL). Most recently, she serves as a leadership member of the Pioneer Network Artifacts 2.0 Advisory Group, Nebraska Culture Change Coalition, and the Developmental Disabilities Aging Coalition.
Lara Cline, MSN, FNP-BC, C-NE, RAC-CT
Director of Care Coordination, Cantex Continuing Care
Lara is the Director of Care Coordination for Cantex Continuing Care Network. In this role, Lara oversees the company’s hospital, physician and alternative payment models initiatives, as well as continues the development and subsequent implementation of the Care Transitions Program. She is the corporate champion for lowering readmissions, INTERACT, and disease management training. Lara earned her B.S. in Psychology at Texas A&M College Station and her B.S.N. at University of Texas Medical Branch Galveston. She earned her Master’s in Nursing as a family nurse practitioner from the University of Colorado Health Sciences Center in Denver where she was selected as for a Robert Wood Johnson Fellowship. She is currently an appointed member of the Clinical Practice Committee for American Health Care Association. Serves on the Texas Healthcare Association Advocacy Committee. She is a life-long learner and patient advocate for quality patient care and the patient experience.
Liz Jensen, RN MSN, RN-BC
Clinical Director, Direct Supply
As a former nurse executive and educator with over 20 years of experience in the post-acute care setting, Liz has worked with hundreds of skilled nursing and assisted living professionals in multiple states to develop strategies and programs to improve care delivery in response to the changing needs of residents and patients. As a nurse executive, her areas of expertise include performance improvement of care delivery systems and programs, clinical education strategies and resource development. She is Board Certified in Gerontological Nursing and her nursing practice experience includes gerontological nursing, dementia care, fall risk reduction, medical/surgical nursing, rehabilitation nursing, infusion therapy and pain management.
Cathy Lipton, MD, CMD
East Region Medical Director, OptumCare Complex Care Management
Cathy Lipton, MD, is an internist and geriatrician serving as East Region Medical Director for OptumCare, the health services arm of UnitedHealthcare’s health plans. Dr. Lipton received her medical degree from Emory University where she practiced as a geriatrician after completing her internal medicine and geriatric fellowship programs. Dr. Lipton was a Medical Director for the Evercare program which evolved into a Medicare Special Needs Plan. She also provides clinical leadership and regional oversight for Optum clinical models serving dual eligible and chronically ill populations as well as patients transitioning from the acute hospital to post-acute settings. Dr. Lipton has been an active member of AMDA/The Society for Post-Acute and Long Term Care for twenty-five years and a consultant to Georgia Quality Improvement Organization for many years.
Donna Hendrickson Fiala, MS
AQAC Consulting, LLC, Assuring Quality and Affordable Care

Keri Hart, MS-CCC/SLP, CHHRP-QT

Loretta Kaes, RN B-C, C-AL, LNHA, CALA
Director of Quality Improvement and Clinical Services, Health Care Association of New Jersey
Dr. Steven Levenson, M.D., CMD
Regional Medical Director, Genesis Healthcare
Dr. Steven Levenson, MD, CMD, is Regional Medical Director, Genesis Healthcare and has spent 41 years providing and overseeing care across the long-term and post-acute care continuum, including assisted living, nursing homes, skilled nursing facilities, and long-term acute care hospitals.
In this webinar, Dr. Levenson will discuss issues related to the indications for opioids and best practices and current thinking about opioid use in acute and nonacute pain.

Dawn Murr-Davidson, RN BSN
Director of Quality Initiatives, Pennsylvania Health Care Association
-
Register
- Member - Free!
- More Information
-
Register
-
Contains 7 Product(s)
Phase 3 of the RoPs goes into effect on November 28, 2019. AHCA has developed resources to help you navigate the new requirements. This package includes resources applicable to Behavioral Health and Trauma Informed Care.
Phase 3 of the RoPs goes into effect on November 28, 2019. AHCA has developed resources to help you navigate the new requirements. This package includes resources applicable to Behavioral Health and Trauma Informed Care. Such as:
- Trauma-Informed Care: How Do I Start
- Trauma-Informed Care Providing Mental Health Services in Long Term Care
- Toward Better Behavior: Yours, Mine, and Everyone Else's
- Sex, Drugs and Rolling Walkers
- Sexuality and the Resident With Dementia
- Behavioral Health and Trauma Informed Care Action Briefs (available in Requirements of Participation Action Briefs)
© 2022 American Health Care Association. All rights reserved.
All Behavioral Health and Trauma Informed Care materials subject to this copyright may be photocopied or distributed for the purpose of nonprofit or educational advancement. The use, photocopying, and distribution for commercial purposes of any of these materials is expressly prohibited without the prior written permission of American Health Care Association.
-
Register
- Member - Free!
- More Information
- Trauma-Informed Care: How Do I Start
-
Contains 5 Component(s)
It is critical to address and mitigate adverse events and potential adverse events. An action plan, otherwise known as a mitigation plan, is a necessary response to adverse events and potential adverse events. For many such events, it is important to respond and start the mitigation process immediately. These tools were initially developed by members of AHCA’s Survey/Regulatory Committee and adapted for assisted living communities to assist providers in addressing adverse events and potential adverse events, documenting and tracking the steps they have taken, and identifying best practices for ongoing improvement. Communities may use different titles or terms than the action plans, such as Director of Health Services instead of Director of Nursing, or service plan instead of care plan. Please adapt the plans to reflect your AL community. Use of these tools does not guarantee regulatory compliance nor mitigate potential liability. Providers should adapt their tools, policies, and processes as needed to ensure compliance with current federal and state requirements and use both professional judgement and the advice of legal counsel in determining whether or how to share these mitigation tools.

How to Register in ahcancalED
Easy as 1, 2, 3 !
click the
 button found in the upper right corner of your screen or follow these three easy steps below!
button found in the upper right corner of your screen or follow these three easy steps below! Step 1

Go to the ahcancalED site at https://educate.ahcancal.org/and log in using the orange button in the upper left hand corner.
Use your usual user name and password that you would use for LTC Trend Tracker or the AHCA NCAL website.
Don’t have one or can’t remember?
Click the log in button and follow the directions found under the search button that reads-“If you need help retrieving your Username or Password, click here”.
*Please note* you must add your member facility name to your login
Once you are in and can see your name in the upper left hand corner, you are ready to go.
Step 2
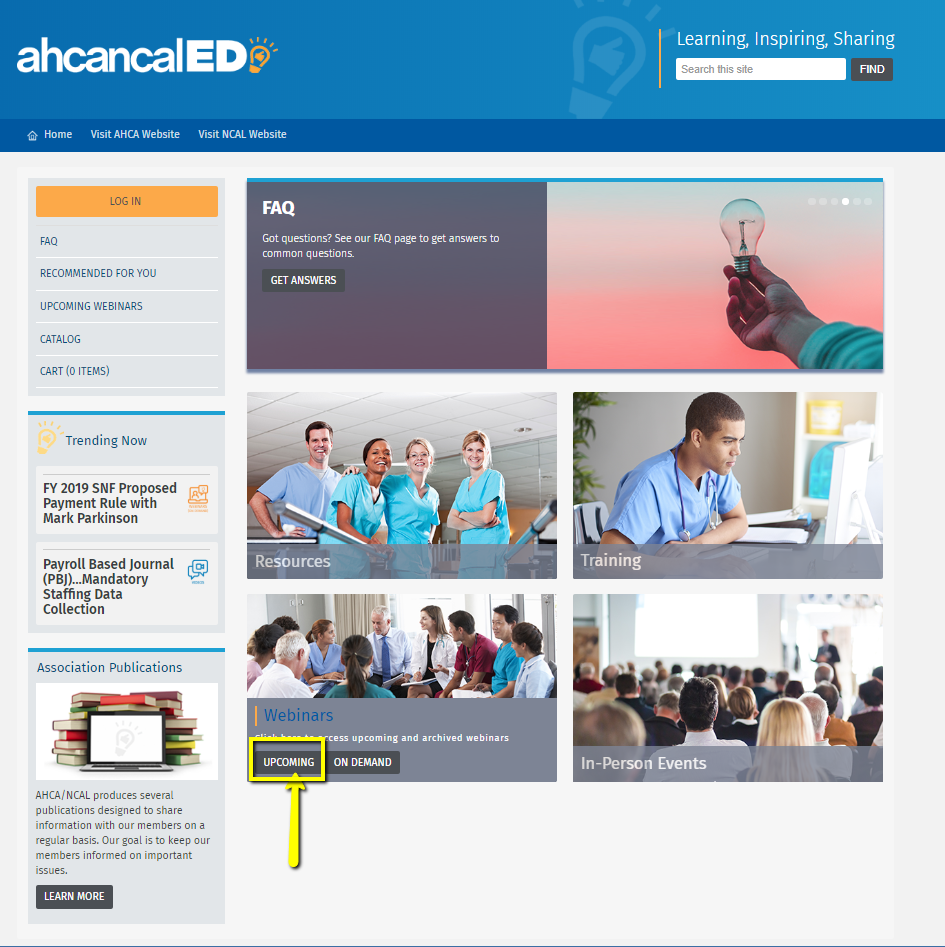
From the home page click on a category (Resources, Training, Webinars or Trending Now) For this demonstration, let’s try hovering over Webinars until upcoming webinars displays.
Under “upcoming webinars” go to a product in which you are interested. Click on the title.
You’ll be redirected to the site where you can register for the product. This allows you to view the overview, handouts or resources associated with that product.
Step 3
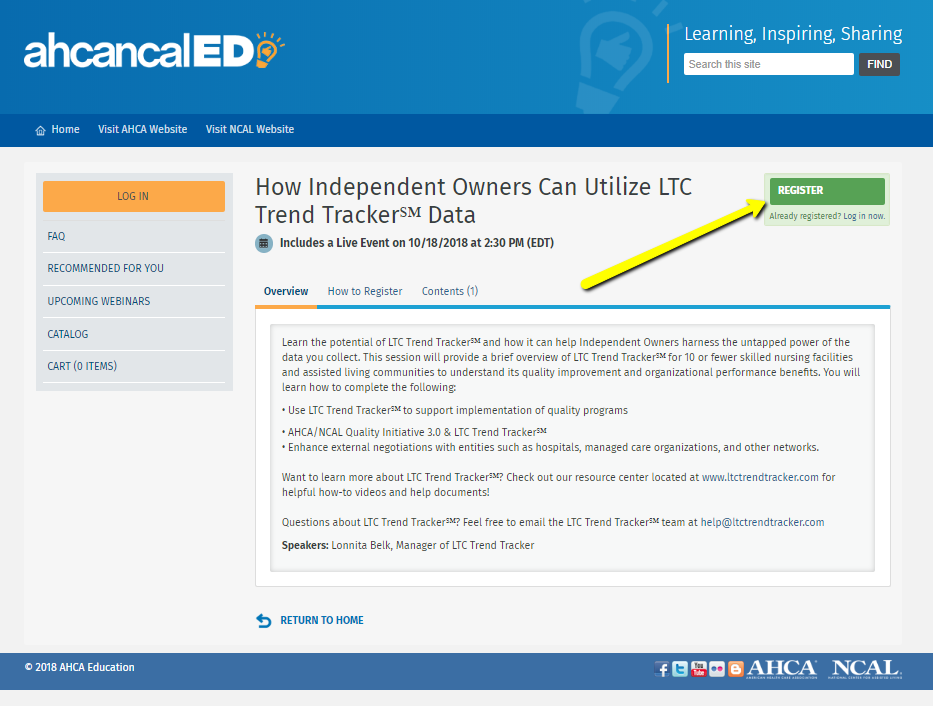
Almost there!
Click the green “register” button.
Fill out the registration details and voila! The products are yours to use indefinitely and can be found in your dashboard.
FYI: after registering, you will be automatically notified when the recording of the webinar is ready.
Need further help? Email us at educate@ahca.org
We’ll walk you through it.
It is critical to address and mitigate adverse events and potential adverse events. An action plan, otherwise known as a mitigation plan, is a necessary response to adverse events and potential adverse events. For many such events, it is important to respond and start the mitigation process immediately.
Examples of adverse events/potential adverse events include:
- Falls (not following the care plan, use of gait belt, one vs. two-person transfers)
- Falls with a mechanical lift
- Elopement
- Allegation of abuse or neglect
- Water too hot
- Smoking (supervised vs. unsupervised, with oxygen, defined smoking area, all about safety)
- Bedrails (entrapment, assessment for use)
- Significant medication errors such as cardiac medications, chemo, insulin, morphine, Coumadin
- Infection Control – outbreaks (e.g. scabies, bedbugs, MRSA, C-Difficile, Noro Virus, Legionella)
- Lack of timely or complete evaluation of a change in condition
- Pressure ulcer – lack of prevention or following prevention measures
- Grievances and resident/tenant council feedback
Objectives:
- Identify adverse events that could potentially have a negative impact on residents/tenants as well as on a community’s regulatory compliance.
- Establish a routine root cause analysis process to identify the specific/source, root cause or causal factor of the problem.
- Create a structured process for developing a mitigation plan to address the adverse event/potential adverse event and minimize similar events for all residents/tenants:
- Complete the Initial Mitigation Action Plan
- QAPI members complete the formal documentation of the Mitigation Action Plan
- Use information learned by sharing results and Plan with the QAPI committee for continued monitoring.
Note: These tools were initially developed by members of AHCA’s Survey/Regulatory Committee and adapted for assisted living communities to assist providers in addressing adverse events and potential adverse events, documenting and tracking the steps they have taken, and identifying best practices for ongoing improvement. Communities may use different titles or terms than the action plans, such as Director of Health Services instead of Director of Nursing, or service plan instead of care plan. Please adapt the plans to reflect your AL community.
Use of these tools does not guarantee regulatory compliance nor mitigate potential liability. Providers should adapt their tools, policies, and processes as needed to ensure compliance with current federal and state requirements and use both professional judgement and the advice of legal counsel in determining whether or how to share these mitigation tools.
© 2022 American Health Care Association. All rights reserved.
All Assisted Living Action Plan Response for Adverse Events materials subject to this copyright may be photocopied or distributed for the purpose of nonprofit or educational advancement. The use, photocopying, and distribution for commercial purposes of any of these materials is expressly prohibited without the prior written permission of American Health Care Association.
You are also encouraged to register for the following free resource:
Tools to Prevent and Address Resident to Resident Mistreatment
-
Register
- Member - Free!
- More Information
-
Contains 5 Component(s)
It is critical for nursing centers and assisted living communities to address and mitigate adverse events and potential adverse events. An action plan, otherwise known as a mitigation plan, is a necessary response to adverse events and potential adverse events. For many such events, it is important to respond and start the mitigation process immediately. These tools were developed by members of AHCA’s Survey/Regulatory Committee. Use of these tools does not guarantee regulatory compliance; nursing centers should adapt as needed to ensure compliance with current federal and state requirements. They are not intended as legal advice and should not be used or relied upon as legal advice.

How to Register in ahcancalED
Easy as 1, 2, 3 !
click the
 button found in the upper right corner of your screen or follow these three easy steps below!
button found in the upper right corner of your screen or follow these three easy steps below! Step 1

Go to the ahcancalED site at https://educate.ahcancal.org/and log in using the orange button in the upper left hand corner.
Use your usual user name and password that you would use for LTC Trend Tracker or the AHCA NCAL website.
Don’t have one or can’t remember?
Click the log in button and follow the directions found under the search button that reads-“If you need help retrieving your Username or Password, click here”.
*Please note* you must add your member facility name to your login
Once you are in and can see your name in the upper left hand corner, you are ready to go.
Step 2
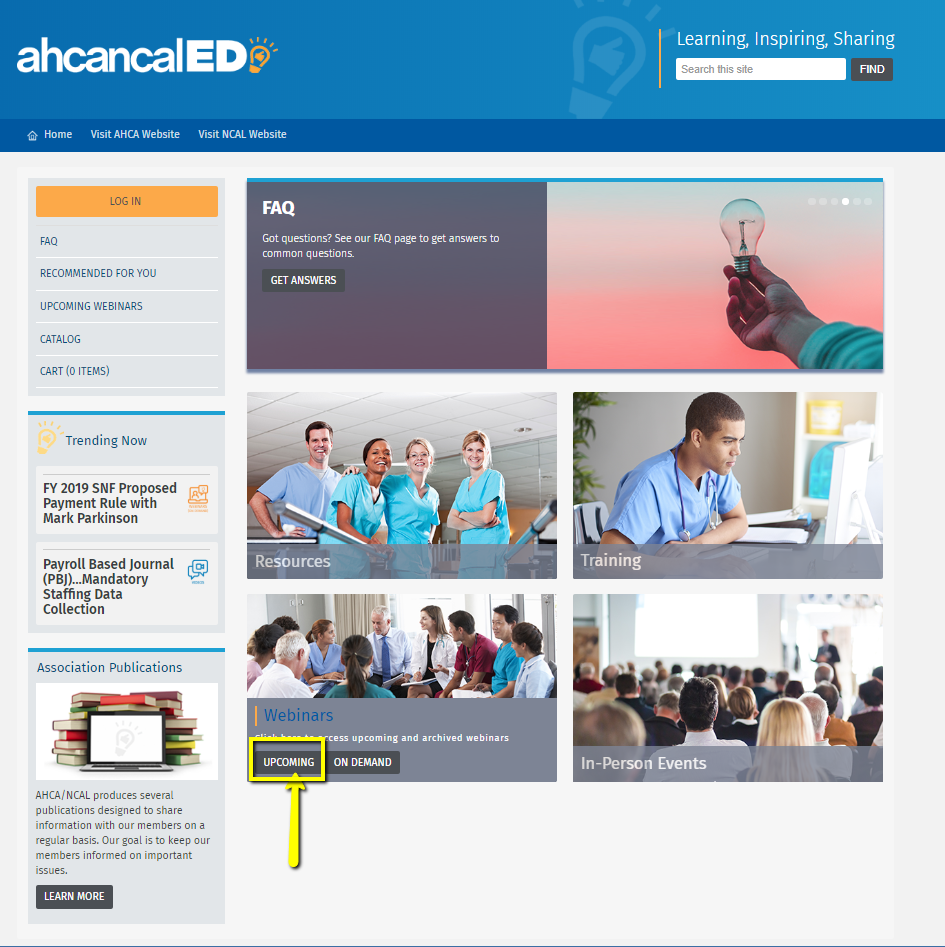
From the home page click on a category (Resources, Training, Webinars or Trending Now) For this demonstration, let’s try hovering over Webinars until upcoming webinars displays.
Under “upcoming webinars” go to a product in which you are interested. Click on the title.
You’ll be redirected to the site where you can register for the product. This allows you to view the overview, handouts or resources associated with that product.
Step 3
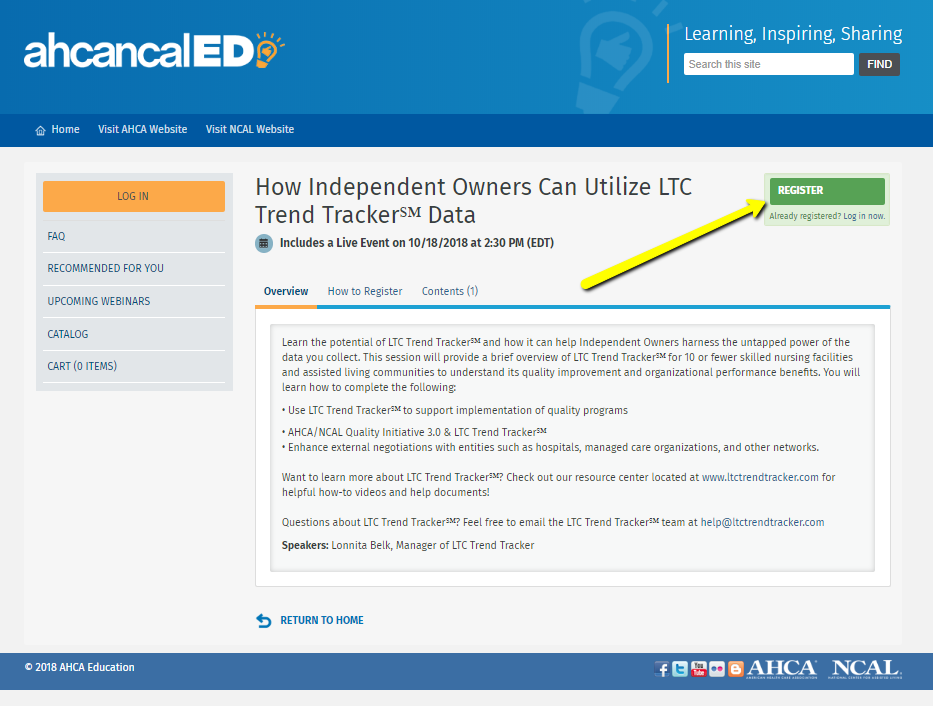
Almost there!
Click the green “register” button.
Fill out the registration details and voila! The products are yours to use indefinitely and can be found in your dashboard.
FYI: after registering, you will be automatically notified when the recording of the webinar is ready.
Need further help? Email us at educate@ahca.org
We’ll walk you through it.
It is critical for nursing centers and assisted living communities to address and mitigate adverse events and potential adverse events. An action plan, otherwise known as a mitigation plan, is a necessary response to adverse events and potential adverse events. For many such events, it is important to respond and start the mitigation process immediately.
Examples of adverse events/potential adverse events include:
- Falls (not following the care plan, use of gait belt, one vs. two-person transfers)
- Falls with a mechanical lift
- Elopement
- Allegation of abuse or neglect
- Water too hot
- Smoking (supervised vs. unsupervised, with oxygen, defined smoking area, all about safety)
- Bedrails (entrapment, assessment for use)
- Significant medication errors such as cardiac medications, chemo, insulin, morphine, Coumadin
- Served/consumed wrong consistency of food or liquids
- Infection Control – outbreaks (e.g. scabies, bedbugs, MRSA, C-Difficile, Noro Virus, Legionella)
- Fluid restriction not managed or monitored by facility, physician parameters not followed
- Lack of timely or complete assessment of a change in condition
- Pressure ulcer – lack of prevention or following prevention measures
- Grievances and resident council feedback
Objectives:
- Identify adverse events that could potentially have a negative impact on residents as well as on a center’s regulatory compliance.
- Establish a routine root cause analysis process to identify the specific/source, root cause or causal factor of the problem.
- Create a structured process for developing a mitigation plan to address the adverse event/potential adverse event and minimize similar events for all residents:
- Review the guidance for determination of avoidable versus unavoidable event
- Complete the Initial Mitigation Action Plan
- QAPI members complete the formal documentation of the Mitigation Action Plan
- Use information learned by sharing results and Plan with the QAPI committee for continued monitoring.
Note: These tools were developed by members of AHCA’s Survey/Regulatory Committee to assist centers and communities in addressing adverse events and potential adverse events, documenting and tracking the steps they have taken, and identifying best practices for ongoing improvement. Use of these tools does not guarantee regulatory compliance nor mitigate potential liability. Providers should adapt their tools, policies, and processes as needed to ensure compliance with current federal and state requirements and use both professional judgement and the advice of legal counsel in determining whether or how to share these mitigation tools.
© 2022 American Health Care Association. All rights reserved.
All Nursing Centers Action Plan Response for Adverse Events materials subject to this copyright may be photocopied or distributed for the purpose of nonprofit or educational advancement. The use, photocopying, and distribution for commercial purposes of any of these materials is expressly prohibited without the prior written permission of American Health Care Association.
You are also encouraged to register for the following free resource:
Tools to Prevent and Address Resident to Resident Mistreatment
-
Register
- Member - Free!
- More Information
Additional Resource available: Social Media Guidance for Nursing Centers and Assisted Living Communities
Additional Resources Available
National Partnership to Improve Dementia Care in Nursing Homes
This National Partnership promotes rethinking approaches that are utilized in dementia care, reconnecting with people using person-centered care approaches and restoring good health and quality of life in nursing homes. Their campaign provides a variety of resources and clinical tools to assist nursing homes achieve these goals.
- National Partnership to Improve Dementia Care in Nursing Homes
- Resources for a Care Giver
- Resources for Persons Living with Dementia
- Resources for Professionals
CMS Hand in Hand: A Training Series for Nursing Homes
CMS, supported by a team of training developers and subject matters experts, created these trainings to address the need for nurse aides’ annual in-service training on important topics.
| Access Date | Quiz Result | Score | Actions |
|---|
Welcome
Log in using your ahcancal username and password.
